Some insects bite humans or animals to feed on their blood and in turn, infect the host with virus, bacteria or a parasite, the resulting diseases are called vector-borne diseases.
A vector-borne disease has three components;
- the infective agent that is responsible for the infection- virus, bacteria or parasite
- the host who is being infected- human or animals
- and the vector or the disease-carrying insect- mosquito or ticks.
Such illnesses include malaria, dengue fever, West Nile disease.
For example, Plasmodium species causes Malaria and it is transmitted by a mosquito bite.
Lyme Disease
Lyme disease is the most common vector-borne bacterial disease in the Northern hemisphere, particularly concerning the US and Europe.
The bacterium causing the disease is the Borrelia burgdorferi and the vector involved is the Ixodes tick.
Borrelia are spiral-shaped bacteria; they belong to the spirochete class, which cause diseases like syphilis, yaws and relapsing fever.
The Ixodes tick is also called the black-legged or the deer tick. These are found in the forest and shrubby areas. The ticks have three life forms; larva, nymph and adult. The tick can be as tiny as a poppy seed to as big as an apple seed.
Mode of infection:
Not all ticks are infective. They can catch the infection by biting an infected deer or a mouse.
A person may develop Lyme disease if an infected tick bites them and remains attached to the skin for 36-48 hours. If the tick is removed within this period, likely, the person will not be infected.
The commonly affected person is a young or an older age male who likes to spend time in nature, such as hunting, hiking, camping, or working in the gardens and backyards.
The younger ticks cause more infections because they are tiny and hard to be spotted, and they are most active during the spring and summer seasons. Conversely, the adult ticks feed during cooler months but are noticed readily because of their size.
Symptoms:
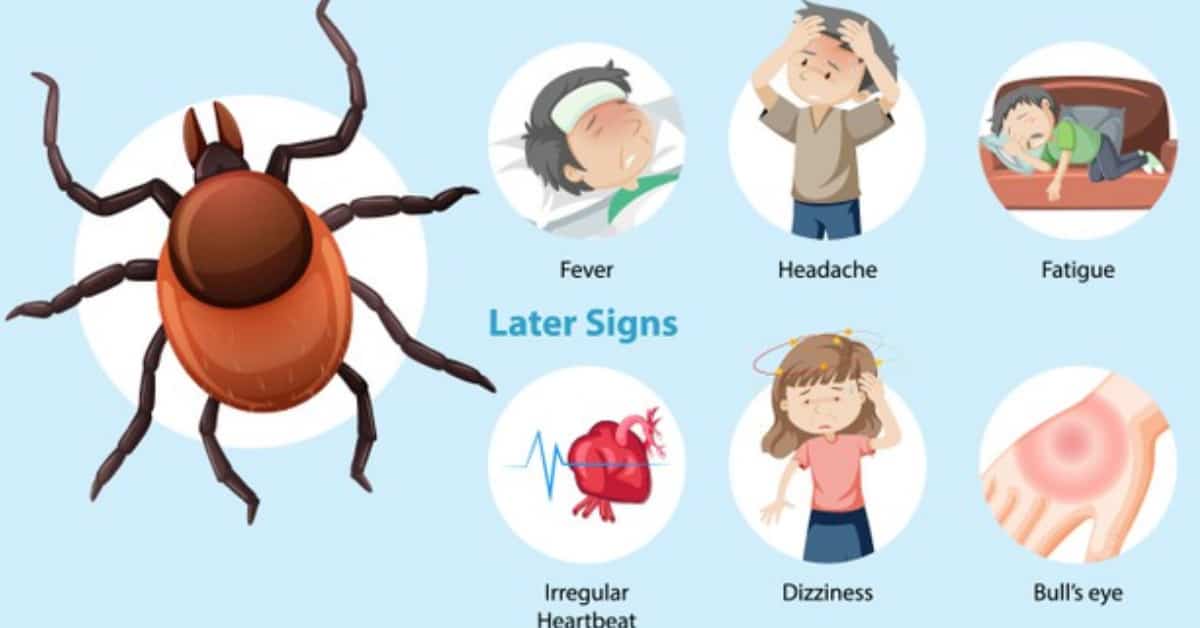
The symptoms of Lyme disease are categorized into three stages:
- Early, localized symptoms:
Symptoms start appearing 3-30 days after the tick bite. There is itching at site of tick bite, fever, malaise, headache, joint pains, swollen lymph nodes, and a characteristic rash.
The skin rash, called the erythema migracans, can occur on any part of the body and usually appears 7 days after infection. It is circular, initially small, measuring 2-2.5 inches and then progressively expanding to up to 12 inches. It can be warm, painful or itchy. A lot of times, it has concentric circles that resemble a bull’s eye target. However, almost 30% of the patients don’t get the rash or fail to see it.
- Early disseminated disease:
The next symptoms appear weeks to months after the first stage. These include:
- Generalized unwell feeling and joint pains
- The bluish red nodules or plaques develop at any part of the body, such as ear lobes, nipples, or genitals.
- The neurological involvementor Neuroborreliosis-affects the brain and the nerves. There’s facial palsy (drooping of one or both sides of face), meningitis (headache and stiff neck), stroke (loss of muscle tone, numbness), shooting pains, and memory loss.
- Cardiac issues or the Lyme Carditis pain- palpitations, and irregular heartbeat.
- Late disseminated disease:
Late symptoms appear if the Lyme disease is not treated during the first two stages. It occurs months to years after the tick bite. The symptoms include joint pains, numbness, mental confusion, memory loss, and difficulty concentrating.
Diagnosis
Lyme disease is diagnosed clinically on the relevant history and examination. The tick bite and the rash, both are the major pointers of the disease. But sometimes, the patient has either not discovered the tick, does not recognize the rash, or remember any part of the incident. So, labs are done to confirm the diagnosis. The most commonly done test is the PCR serology test, which is done in two steps; if first comes positive then the second is done to confirm the diagnosis, else not. This is because of low precision and resemblance to other spirochete diseases (mentioned earlier). The antibodies start appearing after 1-2 weeks in acute stages and after 4-6 weeks for older diseases. The doctor may also order other tests including the Borrelia culture, enzyme immunoassay/immunofluorescence and immunoblot. Clinical diagnosis by the rash is mostly done.

Management:
The management of Lyme disease is focuses on two points, preventing the infection, and treatment depending on the disease stage.
Prevention:
- Keep legs and feet covered while in the woods and shrubby areas
- Use insect repellents on skin and clothes when camping or outdoors
- When back indoors, properly shower and wash the skin and hair
- Put the clothes and gear used in the dryer to kill any pests
If there are any ticks on skin, use tweezers to remove it. Apply the tweezers near its head and remove slowly, otherwise it might break. Check that all of it has been removed. Dispose the tick in rubbing alcohol or stick it to a piece of tape and flush it. Clean the bite area with soap and water or rubbing alcohol.
Areas to look out for :
- Hair and hairline
- Inside and behind ears
- Back of neck
- Armpits
- Inside belly button
- Around waistline
- Groin
- Legs
- Behind knees
- Between toes
Treatment:
Antibiotics are the mainstay of treatment and are given in appropriate doses for long durations to kill the bacteria.
At the 1st stage/rash stage:
Doxycycline is the recommended treatment but not for pregnant women and children less than 8 years old. Alternative antibiotics include amoxicillin or azithromycin.
For the disseminated stages:
Neuroborreliosis: Ceftriaxone, doxycycline, or intravenous benzyl penicillin for 10-30 days.
Arthritis/Carditis: Doxycycline, Ceftriaxone, or Amoxicillin for 14-30 days.
Post-Treatment Lyme Disease Syndrome (PTLDS):
In 1 out of 10 cases, the patient may continue to suffer joint pain, fatigue and memory loss or confusion. This is called the post-treatment Lyme disease syndrome. There is no cure for PTLDS, supportive treatment is recommended. This is seen particularly in cases of late diagnosis or late treatment. An autoimmune factor is suspected to play a role in PTLDS.
Conclusion
Lyme disease is a common vector-borne disease. It is preventable and treatable. Keeping the legs and arms covered while outdoors in shrubs and forests prevent the tick from biting and attaching to the skin. Early recognition of symptoms and the characteristic rash leads to early start of treatment and fuller recovery.
See Also